Simplifying Credentialing for Better Practice Management
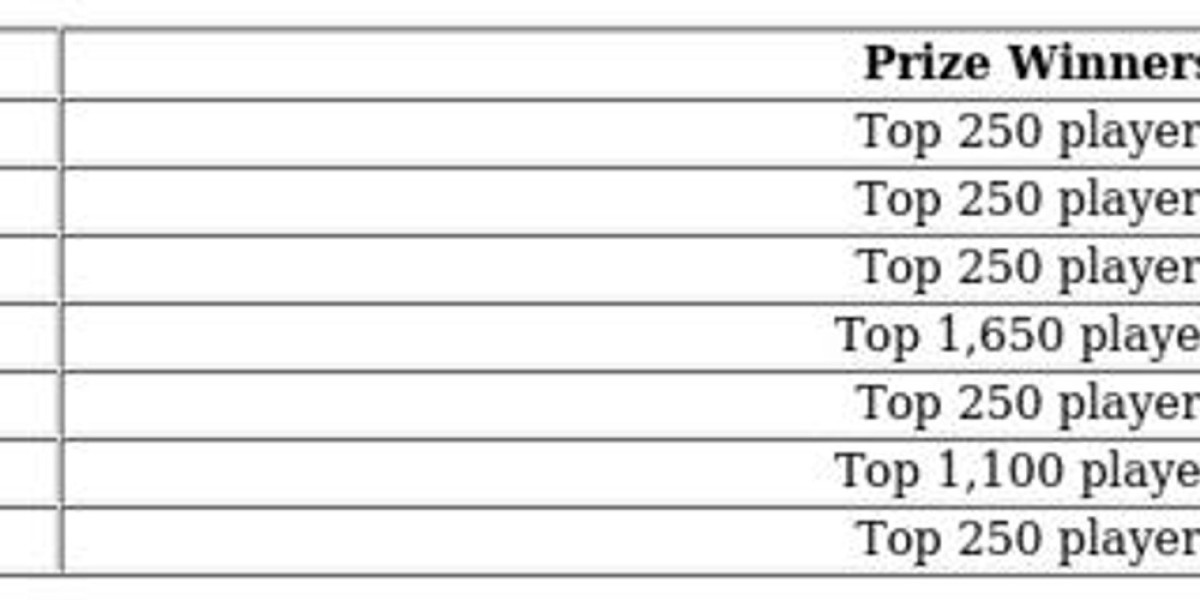
Credentialing is a vital process for any healthcare provider. When handled manually, it can be time-consuming, error-prone, and a burden on internal staff. However, adopting a medical credentialing streamline approach ensures a faster, more organized process. It centralizes documentation, monitors expirations, and eligibility verification process in medical billing providers in compliance with insurance panels and hospital networks.
This efficiency not only speeds up provider onboarding but also reduces the risk of claim denials. Streamlining credentialing aligns the provider’s credentials with insurance requirements—ensuring uninterrupted billing and service delivery.
Accurate Use of POS 11 in Outpatient Claims
Accuracy in place-of-service coding is another critical factor in medical billing.I pos 11 in medical billing designates a service performed in a provider’s office. Misusing or omitting this code can result in claim rejections, underpayments, or audits.
By combining a streamlined credentialing workflow with proper POS coding, providers establish operational integrity. It improves billing turnaround time, reduces denial rates, and enhances transparency across payer communications.